Editor’s note: With our coronavirus coverage, our goal is not to alarm you but to equip you with the information you need. We will try to keep things in context and focus on helping you make decisions. See a list of resources and frequently asked questions here.
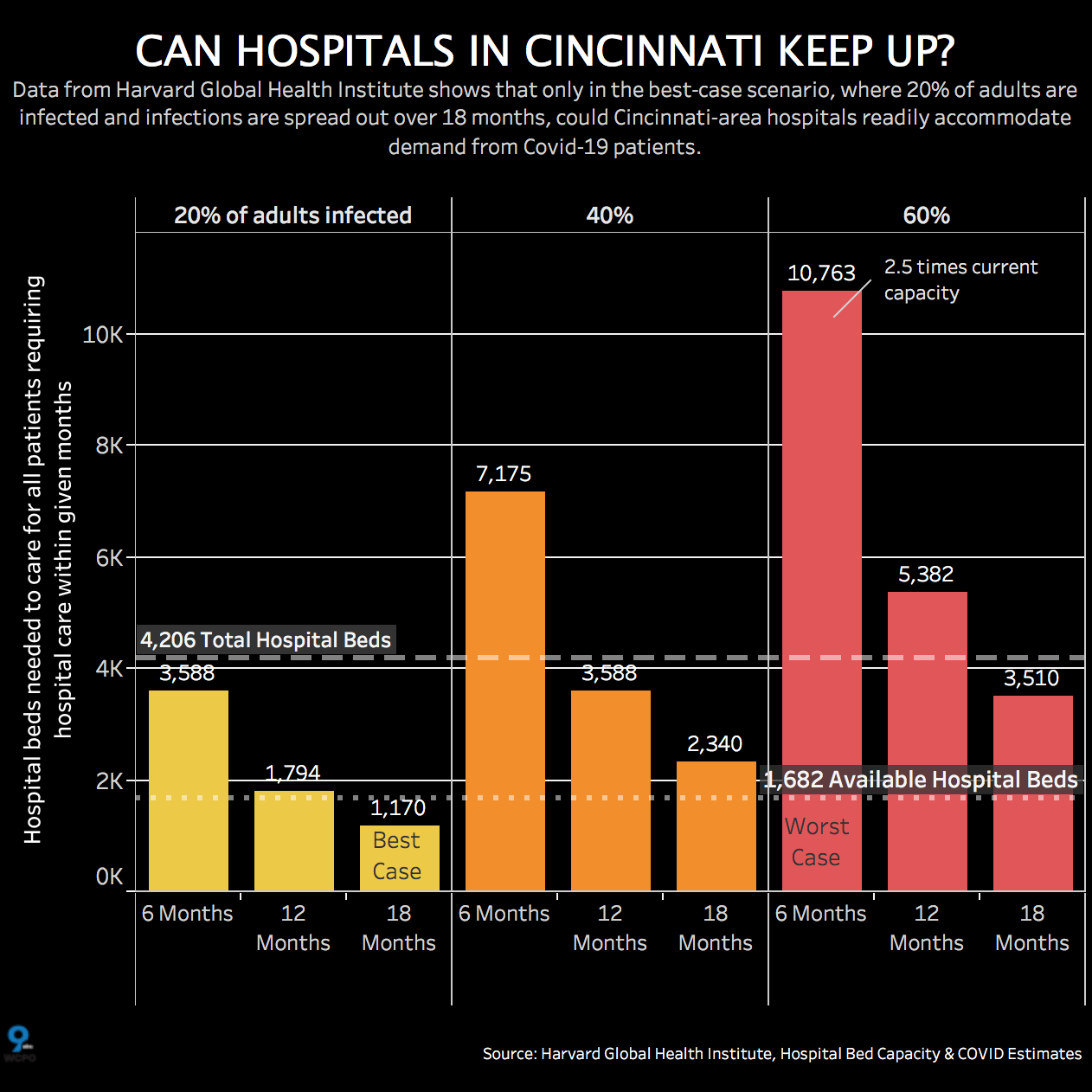
Hospitals across the Tri-State could run out of beds as COVID-19 spreads, putting thousands of lives in danger. As this chart shows, Harvard researchers estimate that a surge could leave the Tri-State up to 6,500 hospital beds short over the next 18 months.
The director of the Ohio Department of Health anticipates running out of hospital beds across the state and says it’s time to build temporary hospitals for COVID-19 patients who need treatment or intensive care.
“You’ll hear more in the news in the days to come about hotels and even dorm rooms being turned into hospital units,” said Dr. Amy Acton.
Out of 18 major hospitals in Southwest Ohio, Northern Kentucky and Southeastern Indiana, there are currently 4,206 beds, according to the American Hospital Directory. Ohio's health director says they are 60 percent full now, after ruling out elective procedures. That leaves less than 1,700 vacant hospital beds.
Acton doesn’t think that’s enough. Neither do Harvard researchers.
“On average, we need hospitals to increase that capacity by 50 percent,” Acton said.
Harvard researchers say if we follow social distancing and stay-at-home orders, we could slow the virus to a 20% infection rate. The Harvard Global Health Institute found that unless we can slow the spread of the pandemic, hospitals could be overwhelmed. The chart helps you see at what point the Tri-State would run out of hospital beds in various scenarios.
Research estimates the number of Tri-State adults who would need hospital beds in the best, moderate and worst-case scenarios – specifically, if the infection rate is 20% or grows to 40% or even 60%.
Theoretically, in the 20% scenario, the Tri-State would have enough beds to handle the load if the cases were spread over 18 months.
But at 40%, we would be nearly 3,000 beds short over six months, and at 60%, more than 6,500 beds short.
Here's the outlook for the states of Ohio, Kentucky and Indiana:
As for building new hospitals, Christa Hyson of The Health Collaborative says, “There’s no firm plans as of yet, but there has been a lot of discussion, you know, involving alternative sites of care. You've probably seen tents of pop-up hospitals outside of existing hospitals. That extends their area of care.
"Other care options could be a pop-up hospital completely separate from that hospital, whether we go into a regional support mode, which would consist of a regional hospital or an alternative-care site.”
So that's why our leaders are telling us if we don’t stay at home and social distance, the hospitals could be out of space and more people could die.
“We know what's coming, because we've tracked what's happened in other states," said Ohio Gov. Mike DeWine.
“We are battling for the health and even the lives of our parents and our grandparents,” said Kentucky Gov. Andy Beshear.
Find more coronavirus/COVID-19 hotlines and resources below:
Ohio
- Department of Health COVID-19 hotline: 833-4-ASK-ODH
- See ODH’s COVID-19 resources here.
Kentucky
- State COVID-19 hotline: 1-800-722-5725
- See the Cabinet for Health and Family Services coronavirus resource site here.
Indiana
- SDH Epidemiology Resource Center: (317) 233-7125 or (317) 233-1325 after hours, or e-mail epiresource@isdh.in.gov
- See more information for coronavirus in Indiana here.
What is coronavirus, COVID-19?
According to the World Health Organization, coronaviruses are "a large family of viruses that cause illness ranging from the common cold to more severe diseases such as Middle East Respiratory Syndrome (MERS-CoV) and Severe Acute Respiratory Syndrome (SARS-CoV).
A novel coronavirus, such as COVID-19, is a new strain that has not been previously identified in humans.
COVID-19 was first identified in December 2019 in Wuhan City, Hubei Province, China and has now been detected in 37 locations across the globe, including in the U.S., according to the CDC.
The CDC reports the initial patients in China have some link to a large seafood and live animal market, indicative of animal-to-person spread. A growing number of patients, however, did not report exposure to animal markets, indicating the disease is spreading person-to-person.
What are the symptoms? How does it spread?
Confirmed cases of COVID-19 have ranged from mild symptoms to severe illness and death, according to the CDC. Symptoms can include fever, cough, shortness of breath.
The CDC said symptoms could appear in as few as two days or as long as 14 days after exposure. It is similar to the incubation period for MERS.
Spread of the virus is thought to be mainly from person-to-person. Spread is between people who are in close contact with one another (within about six feet). Spread occurs via respiratory droplets produced when an infected person coughs or sneezes. The droplets can land in the mouths or noses of people who are nearby or possibly be inhaled into the lungs.
According to the CDC, it could be possible for a person to get COVID-19 by touching a surface or object that has the virus on it and then touching their own mouth, nose or possibly their eyes. This is not thought to be the main way the virus spreads, the CDC said.
The disease is most contagious when people are the sickest and showing the most symptoms.




